What is it?
Appetite is an intrinsic motivator for consuming calories to satisfy the body’s hormonal needs. Hunger and appetite are slightly different in their definition. However, throughout this writing, I will only refer to appetite as a physiological need to consume food rather than the psychological component.
What are the Mechanisms?
The hormonal queues from the body to consume food can be thought of on an axis. The brain’s hypothalamus regulates queues and responds to other hormones to indicate satiety or hunger. I will break down this axis below to show the complex interplay between the brain and the peripheral hormones that dictate appetite.
The hypothalamus in the brain is at the center of function. It receives signals from these four organs to assess the body’s energy availability. The interaction between several or all these organs will determine whether the host can regulate their appetite appropriately. Let’s take a close look at each.
1. Adipose Tissue
Adipose tissue is another name for fat. The two main types of adipose tissue are subcutaneous, fat under your skin, and visceral fat between your internal organs. Fat is an energy source, is also involved in hormone production, and is an insulator and shock absorber.
Leptin. Although ‘fat cells’ were long regarded as passive hosts to store excess energy, the discovery of leptin in 1994 revolutionized our thought process on the role of adipose tissue in the human body. In a healthy scenario, leptin will signal the hypothalamus to induce satiety when fat stores become adequate. Leptin is a long-term indicator of stored energy and is central to our appetite control. This tells us that dysregulation in leptin sensing will harm our ability to regulate appetite. Keep this in mind.
2. The Gut
Several hormones within the gut have been shown to affect appetite regulation. I will break them down individually first and then discuss their interactions.
Ghrelin. Ghrelin is one of the orexigenic hormones, which means it is responsible for making us hungry. When the stomach has been empty for a period of time, or based on circadian eating patterns, ghrelin gets released and travels to the hypothalamus, leading to the hypothalamus release of neuropeptide Y, which initiates hunger and also increases the reward systems of the brain, making food more appealing and even taste better. Ghrelin has been shown to increase the desire for more palatable foods and simple carbohydrates and stimulate a more vivid imagination for food.1
GLP1. When carbohydrates are consumed, the small intestine releases GLP1, responsible for the first phase of insulin response. This means that when GLP1 is released, it creates enough insulin to deal with the amount of carbohydrates consumed rather than allowing the body to over-respond to digested glucose. This allows the body to regulate blood sugar levels and keep them within particular ranges. This has been the target of pharmaceutical companies that have created GLP1 agonists to regulate appetite.
Peptide YY. Peptide YY is another hormone released in the small intestine that responds mostly to protein and fat, indicating the same message to the brain that we are satisfied. It is also an antagonist to ghrelin, and the balance between these hormones is key to regulating appetite. It also seems to have a circadian rhythm, indicating that the times we eat may play an integral role in appetite control.
3. The Adrenals
Your pituitary gland regulates the two adrenal glands that rest on top of your kidneys. During exercise, the adrenals produce the so-called “stress hormone” cortisol, which metabolizes glucose to provide energy.
Cortisol. Cortisol is regulated directly by the hypothalamus through the HPA axis and has been shown to interact directly with insulin and leptin. Acute and low levels of cortisol appear to decrease appetite, but chronic increases in cortisol lead to increased appetite and desire for palatable, hedonic foods. Cortisol can bypass the frontal cortex, our ‘reasoning’ center of the brain, and get straight to the limbic system, leading to more primitive behavior, like the pursuit of immediate pleasure.
4. The Pancreas
The pancreas is located in the upper left abdomen behind the stomach and is involved in hormone production.
Insulin. Insulin is secreted from the beta cells of the pancreas in response to glucose intake or the liberation of glucose from stored sites throughout the body. When inadequate and acute amounts are present, it works peripherally and locally at the hypothalamus to indicate glucose availability and deposits glucose in the body’s cells. Later, when we discuss how it all goes wrong, we will discuss where insulin can be central to losing appetite control.
Somatostatin. Somatostatin is a hormone released from the pancreas that can block insulin and glucagon release. As you can see above, all the peptides and hormones lean towards either satiety or hunger, while somatostatin can sit on the fence. It can increase satiety by slowing gastric emptying but can also increase it by inhibiting CCK and GLP1.
5: The Brain
Malanocite-Stimulating Hormone. Melanocyte-stimulating hormone is a collective name for peptide hormones produced by the skin, pituitary gland, and hypothalamus. In response to ultraviolet (UV) radiation, it has also been shown to lower food intake and increase leptin resistance; it is directly released from the brain and is ONLY released when our eyes are exposed to ultraviolet light.
Where Does Appetite Go Wrong?
Now that you understand the amount of different regulating hormones and incretins that can influence appetite regulation, I will attempt to convey where most of this goes wrong, leading to overeating and obesity. I will also touch briefly on some of the issues considering under eating and eating disorders.
Leptin vs. Insulin. It would seem counterintuitive that chronic high levels of leptin and insulin would lead to poor appetite regulation and overeating. Both can lower hunger when present around the hypothalamus. When first discovered, leptin was sought after as the miracle drug for fat loss. However, scientists discovered that higher levels of circulating leptin are present in overweight and obese individuals. So, what is happening? It seems to be associated with leptin resistance caused by chronic high insulin levels.
In normal concentrations, leptin improves insulin sensitivity, and insulin stimulates the increase of leptin in fat cells. When chronically high, insulin blocks the signal for leptin at the hypothalamus, causing leptin resistance and, therefore, not signaling satiety. Leptin then becomes resistant at the periphery, leading to increased insulin resistance, thus creating a vicious cycle of low satiety and a drop in metabolic rate.2
It also must be recognized that we have not discussed the effects of hyper and hypoglycemia on appetite regulation here, but they also play an essential role.
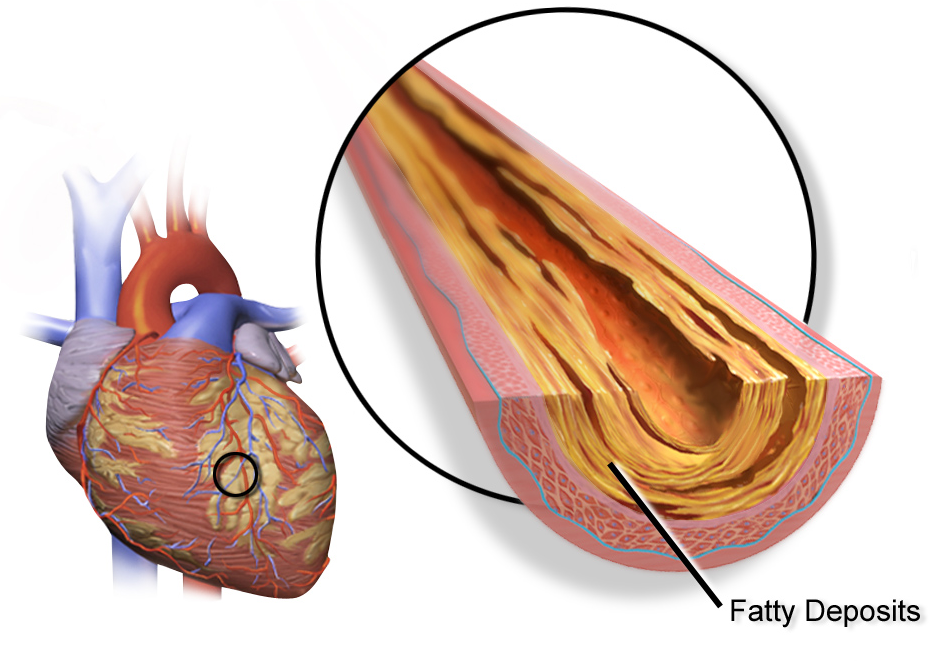
Leptin vs. Cortisol. The relationship between these two hormones is complex and can influence appetite when they run chronically high. I mentioned that a chronic increase in insulin can lead to leptin resistance, and it has been shown that a chronic release of cortisol can lead to insulin resistance due to its constant liberation of glucose and fatty acids.
The above is not a direct link. However, leptin and cortisol connect through the hypothalamus, and research has shown that an acute release of cortisol lowers leptin levels. However, when cortisol levels remain chronically high, it increases leptin resistance and dysregulation of appetite. Also, cortisol can increase triglycerides in the blood, further dysregulating leptin. This leptin resistance increases cortisol as its downregulation effects on the HPA axis are mitigated.
Circadian rhythms. Circadian rhythms are an integral internal clock that regulates processes of the body. It is located in the suprachiasmatic nucleus, which resides in the hypothalamus. Aloof, the hormones above have circadian rhythms, and losing our natural circadian rhythm plays a vital role in appetite regulation. One study showed that sleep deprivation led to a drop in leptin and an increase in ghrelin, causing an increased desire for hyperpalatable (comfort) foods.3 Further studies show that circadian misalignment causes increases in ghrelin, even after we eat, increasing the evidence for the metabolic dysfunction caused by shift work.
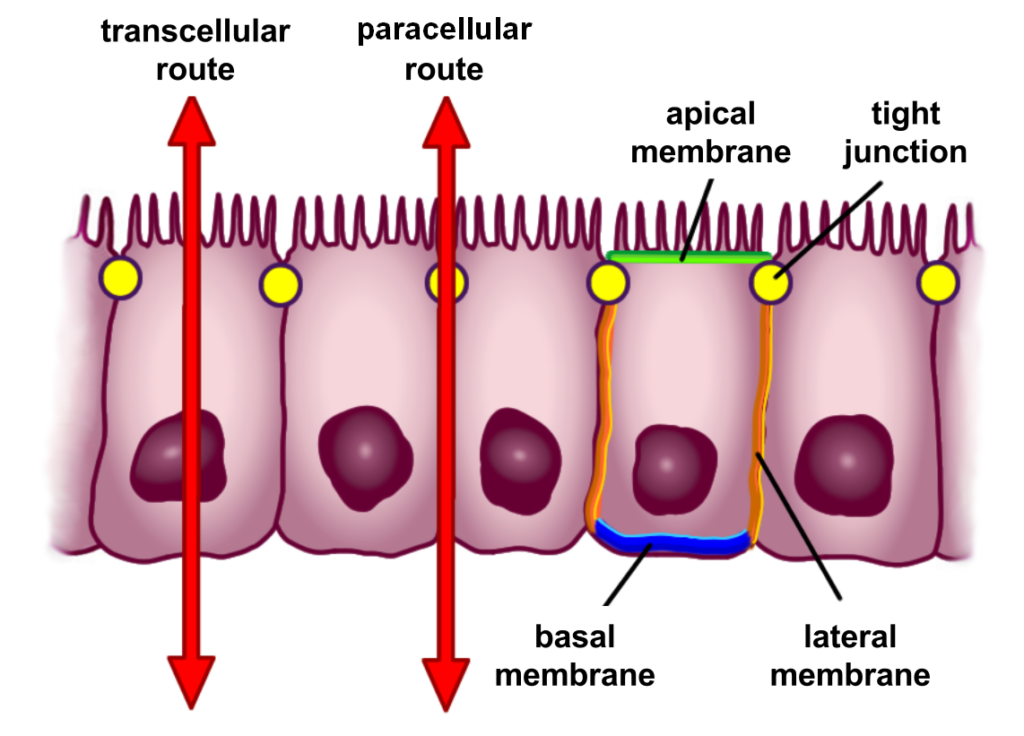
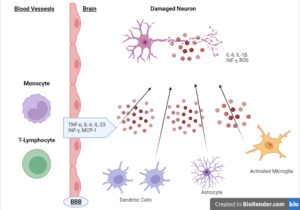
Gut Health. Gut health is far more complex than the mechanisms discussed above, as alterations in gut integrity or dysbiosis seem to affect people differently.
Some studies show that the microbiome’s diversity leads to a lowered level of circulating leptin, and lowered diversity seems to increase it.4 This may indicate that the diversity within our gut may affect appetite positively or negatively, and the practical approaches may differ from client to client. It is also seen in intestinal permeability, where the translocation of LPS into circulation directly affects leptin production in fat cells, meaning it has been shown to lower it, possibly reducing leptin’s ability to influence appetite.
The composition of the bacteria within the gut also seems to affect appetite bidirectionally, but again, it varies from study to study. Short-chain fatty acids, such as acetate, propionate, and butyrate, appear to have positive effects on appetite when not present in chronically high levels, showing that the bacteria that produce these may benefit appetite and weight maintenance.
What are the solutions?
Changes in diet, training, lifestyle, and the use of supplements are effective ways to manage your appetite. Let’s take a closer look at each of them.
Diet. A diet based mostly around high protein and fibrous foods, such as vegetables, has the most positive effects on gut-derived hormones like PYY and CCK. Fiber and protein have also been shown to decrease leptin resistance, at least in animal models.5 Both seem to be stimulated by omega-3 fatty acids, which may indicate that fish could be positive for appetite regulation. GLP1 also responds positively to omega-3 fatty acids. GLP1 also appears to respond favorably to monounsaturated fatty acids like olive oil and avocado.6 This information may indicate that combinations of high protein, and high fiber with combination fatty acids may be the most beneficial nutritional approach to aid appetite regulation.7
Training. Appetite and training are much more controversial subjects. The individual response to acute vs chronic training can vary, and the experience and body weight of the individual are cofactors in the individual response. Studies appear to demonstrate that aerobic work has a more profound effect on appetite suppression than resistance training, and several studies show that aerobic exercise, especially in the overweight population, increases GLP1, CCK, and PYY in some populations. 8
Lifestyle. As discussed in the section on circadian rhythms, you must have adequate and restful sleep to regulate your appetite. In healthy populations without leptin resistance, sleep deprivation lowered leptin levels and increased ghrelin, increasing appetite throughout the day. What about those who were metabolically unhealthy? Sleep deprivation led to increased leptin levels, increased insulin resistance, and increased basal cortisol. This is the triad of increased leptin resistance and voracious appetite.9
Light exposure is a must when we attempt to control appetite. Increases in melanocyte-releasing hormones are only released when our eyes get exposed to ultraviolet light.
Finally, your sleep dictates the circadian rhythm and wake cycle and how you eat. Regular eating timing is integral to regulating appetite; variations increase appetite. Ghrelin responds predictively to the times you regularly eat, and those who front-load their food consume the most in the morning and have the best appetite control.10 Takeaway: Adequate sleep, somewhere between 6.5 to 8 hours, is necessary for appetite regulation, but the mechanism of action varies depending on your health status. Eat food simultaneously daily, front-loading your food intake as much as possible.
Supplements. The following supplements will attempt to break this axis of appetite, affecting different stages to regain control of your feeding habits.
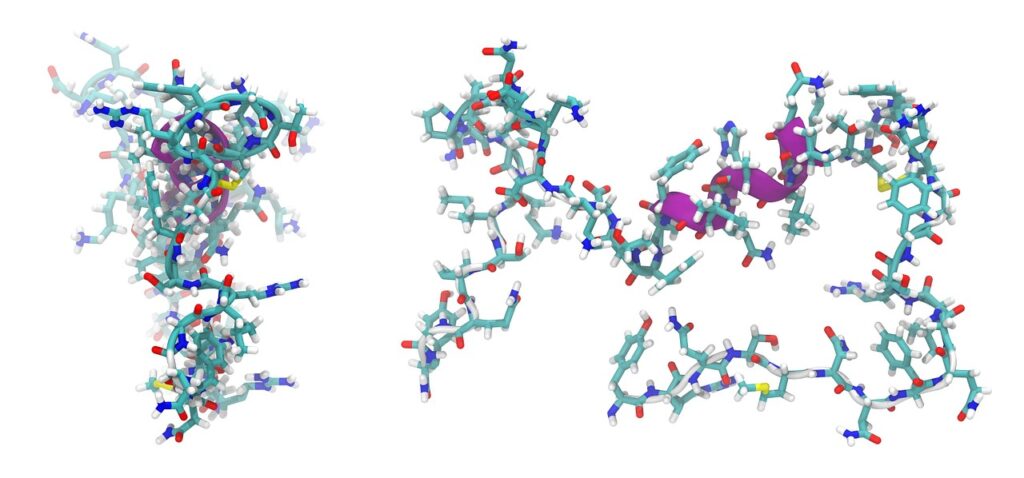
Omega 3. Omega 3, EPA, and DHA, have been shown to affect the axis in many ways. First, it has been shown to lower leptin levels in those where it is chronically elevated.11 As discussed earlier, insulin resistance plays a central role in leptin resistance, and omega 3s have been shown to aid in desensitizing insulin.12 It has also been shown to lower our perception of stress, lower cortisol, and increase GLP1. 13 Adding to this, it is one of the potent fats for stimulating CCK. Dosage: 2-4g of combination EPA/DHA in split doses.
Glutamine. The amino acid glutamine has been used for decades for its positive effect on gut integrity. It also appears to positively impact appetite, blood sugar regulation, GLP1, leptin, and lowering triglyceride levels, which can block leptin from reaching the brain. 13 It also has potent effects on increasing CCK. Dosage: 10-20g daily.
Magnesium. Magnesium targets the axis in many ways. A meta-analysis found that increasing the amount of CCK in the gut leads to increased feelings of satiety and lower calorie intake.13 Magnesium also indicates a positive effect on insulin resistance and energy production.14 Finally, it also helps to lower cortisol.15 Dosage: 300mg-500mg a day in divided doses.
Berberine. The alkaloid berberine has been shown to affect blood sugar regulation positively. Some studies even show it is as effective as metformin at regulating blood sugar and has the added benefit of lowering lipids, which play major roles in leptin resistance.16 It has also been shown to increase GLP1 in many studies17 Dosage: 1000mg to 2000mg daily, divided doses, with meals.
Quercetin. Quercetin has been shown to positively affect appetite-regulating hormones by its digestive support properties and ability to regulate uric acid, insulin resistance, and leptin levels.18 It has also shown positive effects by increasing GLP1 and lowering triglycerides.19 Dosage: 1200-2400mg a day in divided doses.
Fiber. Soluble and insoluble fiber can increase CCK and GLP1 and lower leptin resistance effectively. 22 Studies in humans tend to be more subjective than directly analyzing the hormones and incretins; however, animal studies demonstrate the effects. SCFA, the byproduct of carbohydrate fermentation, has also been shown to affect the peptide YY increase positively. Dosage: 5g to 10g daily of combination fiber sources.
Conclusion
Appetite regulation is a complex interplay of physiological and psychological components. There is a dynamic crosstalk between different hormones and incretins that all play back into the hypothalamus to determine our drive to consume energy. Knowing the mechanisms at play allows us to use the most effective science-based approach to target the feeling of satiety.
Front-loading calories with mostly protein, fat, and fiber makes the most sense here, along with consistent meal timing, appropriate sleep patterns, and combination fatty acid therapy. This approach, along with the neutraceuticals mentioned, should give our clients the best chance to succeed.
Reference Links :
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5373497/
2. https://www.spandidos-publications.com/10.3892/etm.2020.9327#b13-etm-0-0-09327
3. https://pubmed.ncbi.nlm.nih.gov/15602591/
4. https://microbiomejournal.biomedcentral.com/articles/10.1186/s40168-021-01093-y#ref-CR35
6. https://nutritionandmetabolism.biomedcentral.com/articles/10.1186/s12986-016-0153-3/tables/2
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6164815/
9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8138234/
11. https://www.sciencedirect.com/science/article/pii/S0271531720305674
13. https://www.mattioli1885journals.com/index.php/progressinnutrition/article/view/9081
14. https://pubmed.ncbi.nlm.nih.gov/28526383/
15. https://www.ncbi.nlm.nih.gov/books/NBK507250/
16. https://www.sciencedirect.com/science/article/pii/S0753332223005437
18. https://www.sciencedirect.com/science/article/abs/pii/S1875536409600388