What is it?
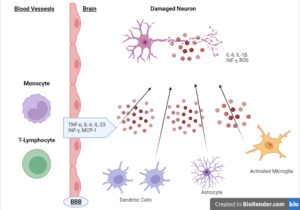
Neuroinflammation is an injury to the brain or central nervous system strongly associated with the microglia within the brain. We often think of the brain as a bunch of neurons, but there is so much more, as neurons only represent 15% of the total brain volume. When immune cells become overactive, they are pulled away from other tasks to deal with the inflammatory cascade.
Neuroinflammation presents itself in three stages: Transient Inflammation, Chronic Inflammation, and Primed Glial Cells. Each of these stages presents with very different signs and symptoms, as follows:.
Transient Neuroinflammation (Easy Solution)
- Brain fog
- Variations in mental speed
- Reduced brain endurance
Chronic Neuroinflammation
- Depression
- Inability to concentrate
- Sleepiness and lack of motivation
Primed Glial Cells
- Unresponsive depression
- Fall apart under triggers (discussed below)
- Seizures
Neuroinflammation can present in many ways, but we need to understand the client’s stage and what it represents. Brain inflammation from poor lifestyle and food choices is likely transient and simple to correct. However, if you have a client with primed glial cells from head trauma, it is completely life-changing, and all aspects below need to be addressed.
What are the causes?
Several different factors can cause neuroinflammation. Here are a few:
Head trauma and TBI. This is most likely to be the cause of chronic and primed glial cells and may not appear until years after the initial trauma. It is called the “Second Hit Theory” of neuroinflammation. It means that you or your client may have experienced a head injury, but the next insult, quite possibly a smaller insult, may exacerbate symptoms. We see those with multiple TBIs have increased odds of neurodegeneration and cognitive decline.
Chronic Stress. Chronic stress can induce transient neuroinflammation and exacerbate the condition if already present. Although it may appear that stress is a cop-out for most conditions, it is prevalent in this one.
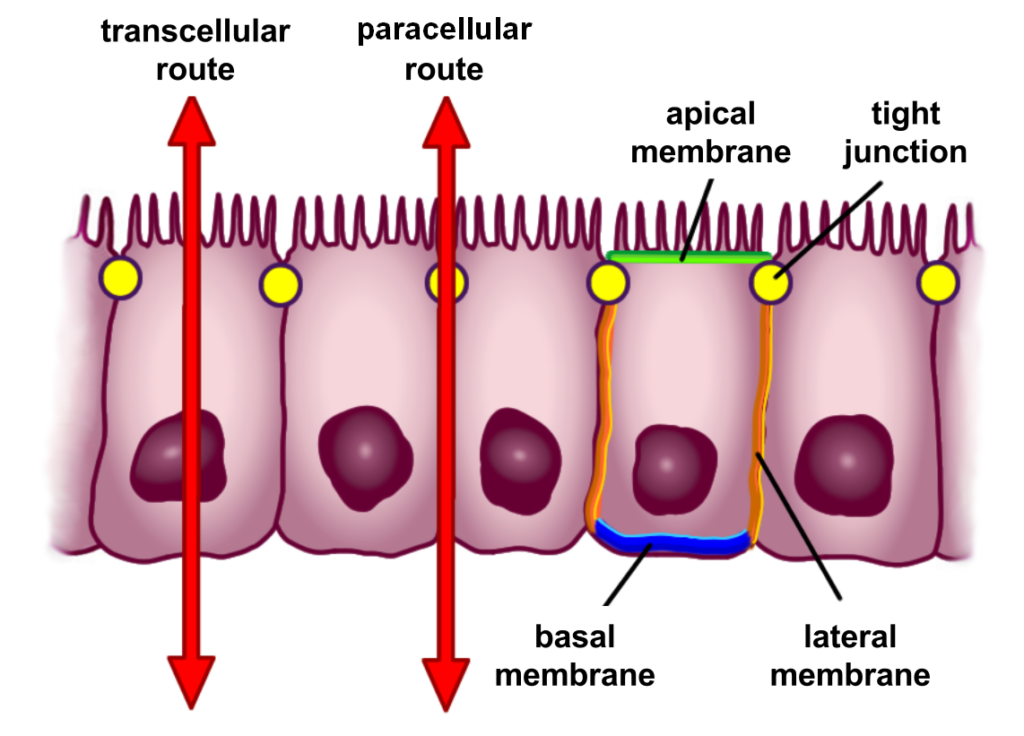
Alcohol and Drug Use. Alcohol and drugs are significant contributors to brain inflammation and have distinct effects on different parts of the brain. The cerebellum is particularly sensitive to ethanol, leading to the poor motor control seen when too much alcohol is consumed. For those suffering from different signs of neuroinflammation, it is essential to remove alcohol as much as possible. Alcohol can also break down the blood-brain barrier, which controls things that enter the brain, and unwanted molecules enter the brain when this breaks down.
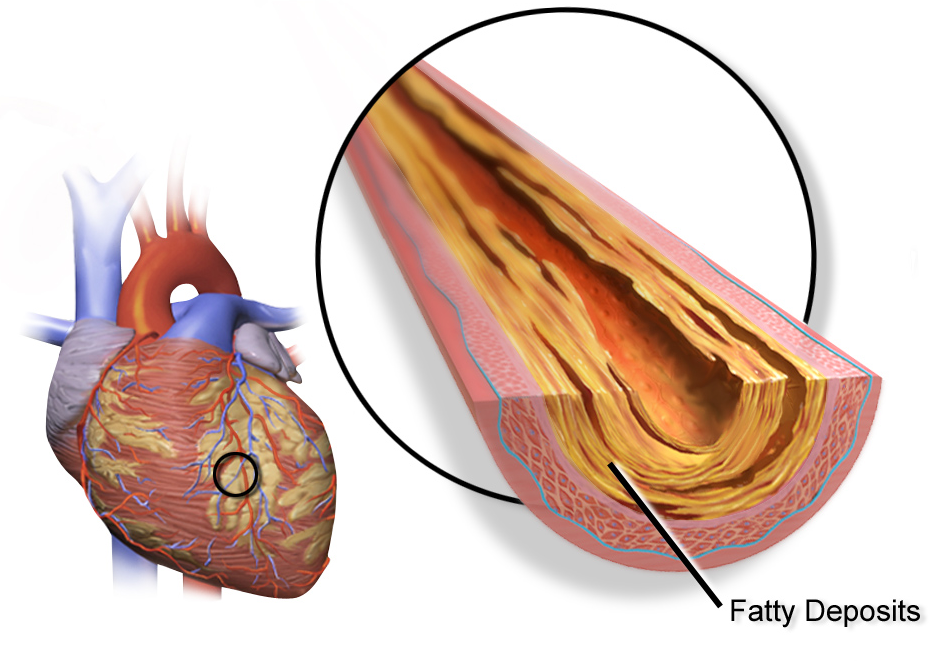
Systemic Inflammation. Systemic inflammation, especially from the gut and the liver, has feedback mechanisms to the brain through the vagal nerve, creating a highway of inflammatory stimulus in the brain. We see this in non-alcoholic fatty liver disease, where one of the major complaints is depression and anxiety. Poor gut health and intestinal permeability also contribute through this mechanism and the transfer of gram-negative bacteria (LPS) from the gut that can break down and pass the blood-brain barrier.1
Blood Sugar and Obesity. Blood sugar variation may significantly contribute to brain inflammation and is a huge compounding factor for those with brain inflammation. High and low blood sugar levels increase the proinflammatory cytokine IL6, and inflamed brains require higher glucose demands, leading to drops in blood sugar. Fat cells can increase systemic and localized inflammation within the brain through the immune reaction, particularly in the visceral, white fat tissue. High levels of insulin, caused by increased blood sugar, further cause inflammation in the brain through the RAGE reaction.2
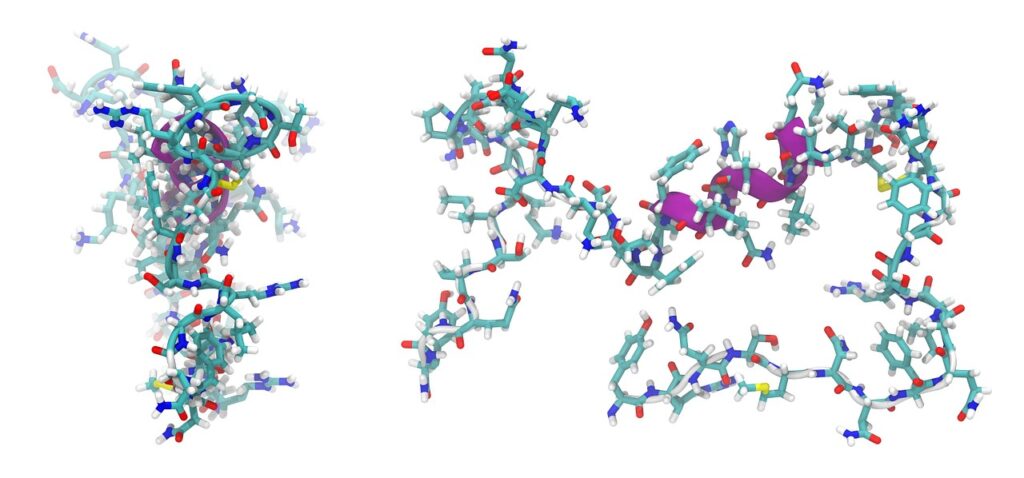
Protein Triggers. Specific proteins, such as gluten and dairy, can trigger neuroinflammation and are one of the most likely things to compound already inflamed brains. Gluten has a protein strand very similar to that of the cerebellum portion of the brain, and antibodies against gluten can also attack the cerebellum when gluten is consumed. People may notice that when they consume specific food protein, they get brain fog, or their mood is affected.3
What are the solutions?
When glial cells become activated in response to a pathogen or damage, they quickly shift to an M2 state, which is pro-inflammatory. When the response becomes chronic or sustained, it can shift more to an M1-dominant state. Our job is to bring them to a more M2, anti-inflammatory state through diet, lifestyle, and supplementation. There is no pill for this condition, and if your client has primed glial cells, adherence to the plan is integral for normal function. Let’s take a closer look at what can be done:
Diet. As mentioned above, dietary approaches are one of the most important factors when attempting to control and subdue neuroinflammation. Elevated blood sugar and insulin are key culprits in the continued assault on the brain. The first stage is a controlled carbohydrate diet, with whole foods and avoiding protein triggers such as gluten and dairy. Controlling carbohydrate intake will allow for continued brain supply without large, dangerous blood sugar and insulin increases.
More aggressive diets, such as the ketogenic diet, can be utilized as ketones shift glial cells from an M1 to an M2 state, replacing glucose as an energy source.
The combination of sugar and saturated fat is the perfect storm for perpetuating neuroinflammation, so it’s essential to control carbohydrates and change the fat sources to healthy fats such as olive oil, avocado, and fish.4
Training. Exercise in any capacity will be an essential part of any program to dampen neuroinflammation.5
Aerobic and resistance training have both been shown to affect neuroinflammation positively. The program’s intensity must be led by the extent of the symptoms. Those with chronic neuroinflammation need to be drip-fed exercise, and the intensity increases over time because too much can lead to an inflammatory state and increased symptoms.
Analyze symptoms, start with low intensity, and build over time.
Lifestyle. Two main components of lifestyle, sleep and stress, are integral to resolving this condition, as follows:
1. Sleep. Sleep is essential for general health and most ailments and conditions, particularly in this situation. Even without previous neuroinflammation, mice with poor sleep quality have been shown to develop low-grade neuroinflammation without the other compounding factors mentioned.
As neuroinflammation cannot be seen under scan, these studies cannot be done in humans due to the need for an autopsy. However, we do see that those who have poor sleep length and quality are known to have glucose and insulin dysregulation. Prioritize sleep as a critical element of your protocol if you wish to overcome neuroinflammation.
2. Stress. Chronic activation of stress pathways and hormones has been shown to increase neuroinflammation 6, and methods to lower choric stress have been demonstrated to have positive effects. Research indicates that stress reduction modalities such as meditation and breathwork can positively affect brain function. Meditation, breathwork, Tai chi, and yoga can also positively affect inflammatory states in multiple conditions.6
Supplements. Here are five powerful supplements that can help with neuroinflammation:
1. NAC/glutathione. NAC and glutathione are powerful antioxidants that can quench oxidative stress in the brain, allowing for the dampening of the “fire.” They can also support mitochondrial function in the brain and lower inflammation.7 Dosage: NAC- up to 2400mg daily in divided doses.
2. Curcumin. The polyphenol curcumin has been shown to affect systemic and brain inflammation positively and may have multiple mechanisms of action. It has positive effects on the gut, liver, and brain. It lowers inflammation, improves gut diversity, and protects neurons.8 Dosage: 1000-2000mg a day in divided doses.
3. Fish oils (DHA/EPA). DHA helps construct neurons within the brain and is depleted when there is neuroinflammation, as it is liberated to support controlling the blaze. Increasing DHA, in particular, has positive effects on modulating neuroinflammation.9 Dosage: 1000-2000mg a day of DHA.
4. Resveratrol. Resveratrol is another polyphenol shown to have positive effects in multiple mechanisms. Like curcumin, it can have systemic anti-inflammatory and antioxidant effects but can also cross the blood-brain barrier and positively affect the brain.10 Dosage: 1000mg a day in divided doses.
5. Short-chain fatty acids (butyrate). These amazing molecules, created in the gut from the fermentation of fiber in the large intestine, have been shown to have far-reaching effects outside of the gut. They have been demonstrated to positively affect energy production and kidney, liver, and brain function. Dosage: 1000mg a day in divided doses.
Conclusion
As with many conditions, neuroinflammation is not localized to the brain. Many other factors, from gut dysfunction to NAFLD and systemic inflammation, may play a major role in the associated symptoms. Addressing other factors with the abovementioned approaches may be necessary, but these strategies are scientifically backed and accredited to help you achieve optimal brain function.
Reference Links :
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2789209/
2. https://www.frontiersin.org/articles/10.3389/fnins.2021.687157/full
4. https://www.frontiersin.org/articles/10.3389/fimmu.2018.02067/full
7. https://pubmed.ncbi.nlm.nih.gov/10543018/
8. https://pubmed.ncbi.nlm.nih.gov/28204864/