What is it?
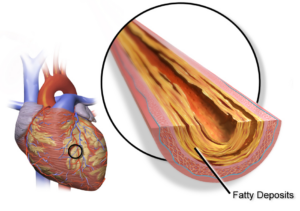
Metabolic-associated fatty liver disease (MAFLD) is a relatively new-regarded metabolic condition where fat accumulates in the liver without the presence of alcohol abuse. It’s estimated that up to one in three individuals who are overweight have nonalcoholic fatty liver disease, but it has been found in those who are lean.
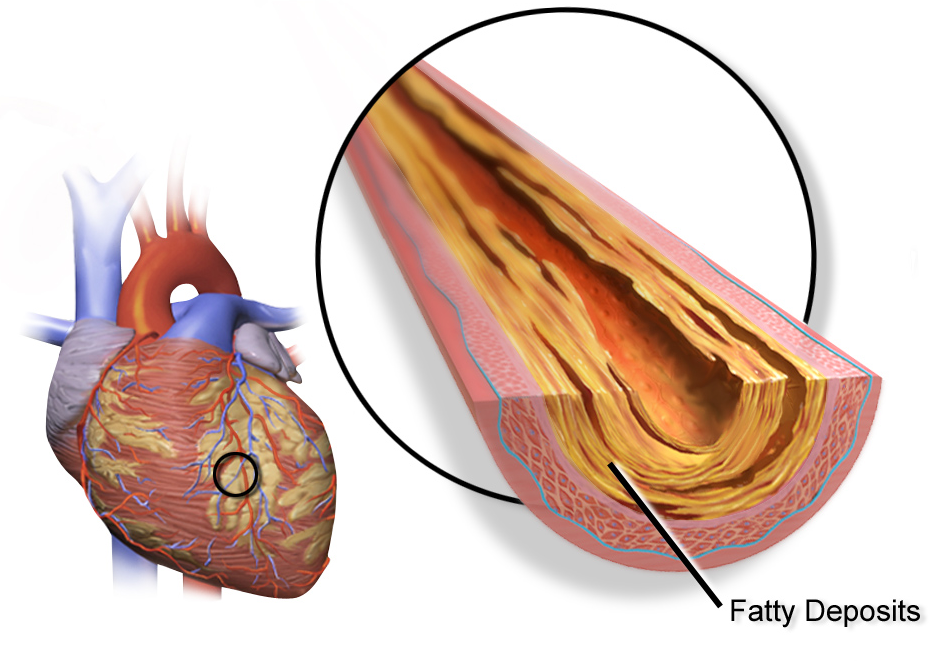
MAFLD can be the beginning of a progression into more severe liver dysfunction, such as nonalcoholic steatosis (NASH) and liver cirrhosis, so it must be taken seriously. This disease does not just contain itself in the liver, as it is associated with other diseases, including cardiovascular disease and cancer.
Some of the symptoms of MAFLD may be surprising, ranging from subclinical depression and anxiety to cognitive decline and chronic pain.
What are the mechanisms?
The first step in managing MAFLD is to determine the causes. Here are three of the major ones:
Diet: Because the score to determine if you have MAFLD includes triglycerides, BMI, insulin, AST, and ALT, diet is the predominant theory for why MAFLD develops. High caloric, high fat, and high sugar diets and other poor eating habits lead to increased insulin resistance and poor mitochondrial function in the liver, further exacerbating the issue. High-fructose diets have also been shown to increase the speed of disease progression.
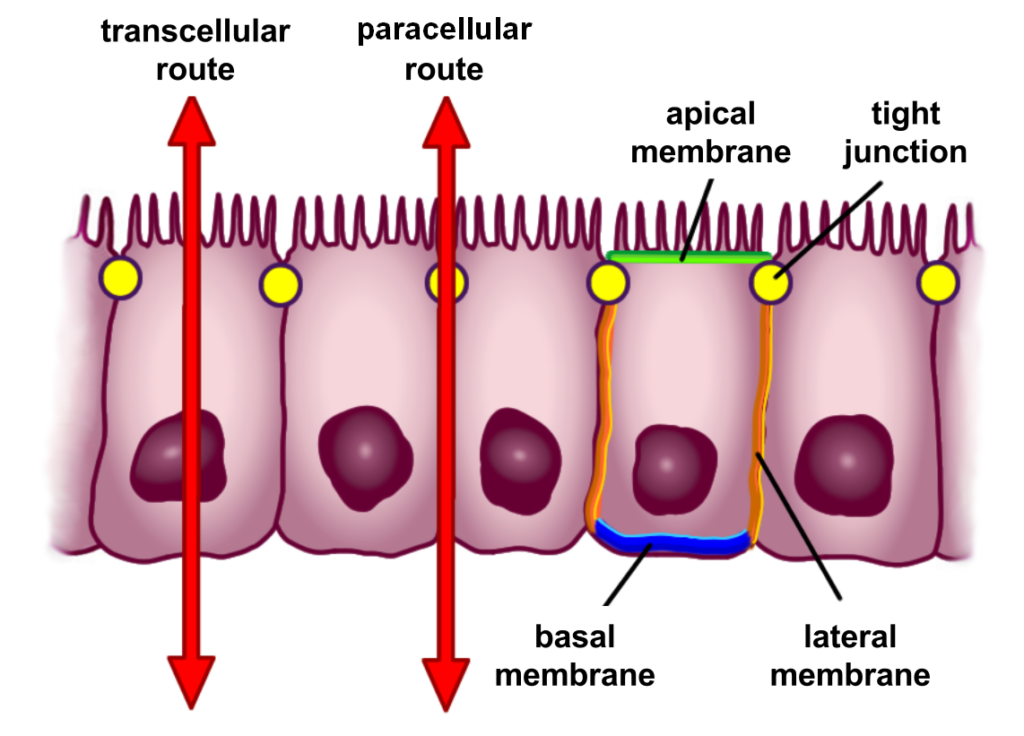
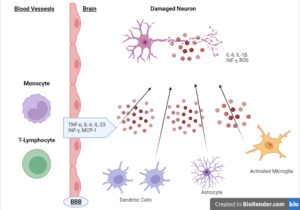
Gut Health: It was initially thought that MAFLD was a “Two-Hit Theory,” where too much fat entering the liver and insufficient removal combined with increased inflammation and oxidative stress were the culprits. This theory has been expanded to the ‘Multiple-Hit Theory of MAFLD’, where multiple systems are responsible for this condition.
Gut and intestinal permeability are significant contributors to MAFLD. When LPS (lipopolysaccharide) from gram-negative bacteria gets into the portal vein, it is taken directly to the liver. In the liver, it attaches to receptors called toll-like Receptor 4, which leads to excess inflammation. This explains why dysbiosis and intestinal permeability are key contributors to MAFLD and could be why we see it in those who are not overweight.
Mitochondrial Dysfunction: Mitochondrial dysfunction within the liver has been associated with the progression of the disease due to its downregulation of oxPHOS during overexposure to fatty acids. This leads to increased ROS and inflammation within the liver.1
What are the solutions?
Changes in diet, exercise, and the use of supplements have shown promise in addressing MAFLD. Let’s take a closer look.
Diet. No single tablet is available for this condition, and diet is the most effective method for lowering intrahepatic triglycerides. Specifically, a short-term VLCD (2-4 weeks) followed by a hypocaloric Mediterranean-style diet thereafter is beneficial.
Exercise. Combining aerobic and resistance training positively affects MAFLD. Even aerobic work has been shown to lower MAFLD even without weight loss on a eucaloric diet. A eucaloric diet is when you consume the same number of calories you expend.
Supplements. The following supplements have been shown to help manage MAFLD:
Choline: Choline-deficient diets have been shown to induce MAFLD. Dosage: Choline at 2g per day is effective.
Vitamin E: Vitamin E has been shown to have clear benefits in lowering liver enzymes and fatty deposits. Dosage: Doses of up to 1200iu are beneficial. Tocotrienols, a derivative of vitamin E, have also been shown to have similar effects at 300mg daily.
NAC: NAC has not been shown to lower hepatic fatty deposits but has been shown to lower liver enzymes in many studies. Dosage: Doses of up to 2400mg have been used.
Nigella Stevia (Black Cumin Seed Oil): Nigella stevia has wide-reaching effects on the liver, including lowering enzymes, liver fat accumulation, and markers of inflammation. Dosage: Up to 2 grams a day can be used.
Curcumin. Curcumin is used for many inflammatory conditions, including neuroinflammation and UC. Curcumin affects the liver by lowering liver enzymes. Dosage: Up to 2 grams daily can be used.
Berberine: Many studies have used berberine to regulate blood sugar, and we understand that insulin resistance is one component of MAFLD. Berberine also has the effect of being an antimicrobial within the gut and may lower liver fat accumulation and body weight. Dosage: 1500mg a day in divided doses with food is effective.
Omega 3: Omega 3 has similar anti-inflammatory effects to curcumin and is effective with MAFLD. Dosage: 1-2 grams of combined EPA/DHA are appropriate here.
Probiotics: Probiotics are effective at controlling gut dysbiosis, one of the significant factors in the multiple hit theory. This may explain why probiotics may lower liver enzymes and affect insulin.
Conclusion
There are clear and scientifically validated nonpharmaceutical interventions for treating MAFLD, and these should be the first step taken when dealing with this disease. Taking your nutrition and training seriously, in combination with supplements, has been shown to reverse this condition completely.