What is it?
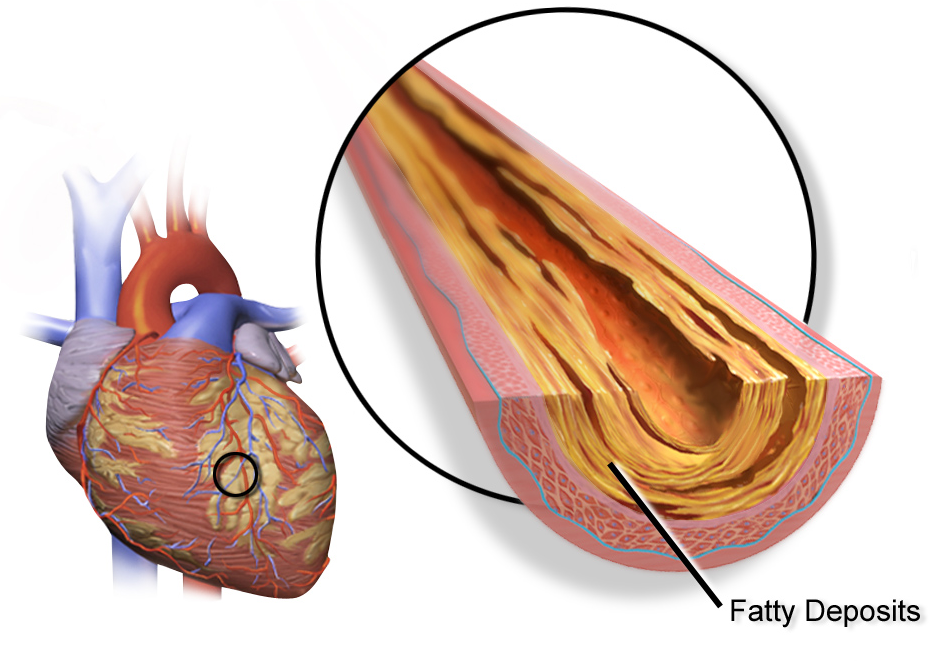
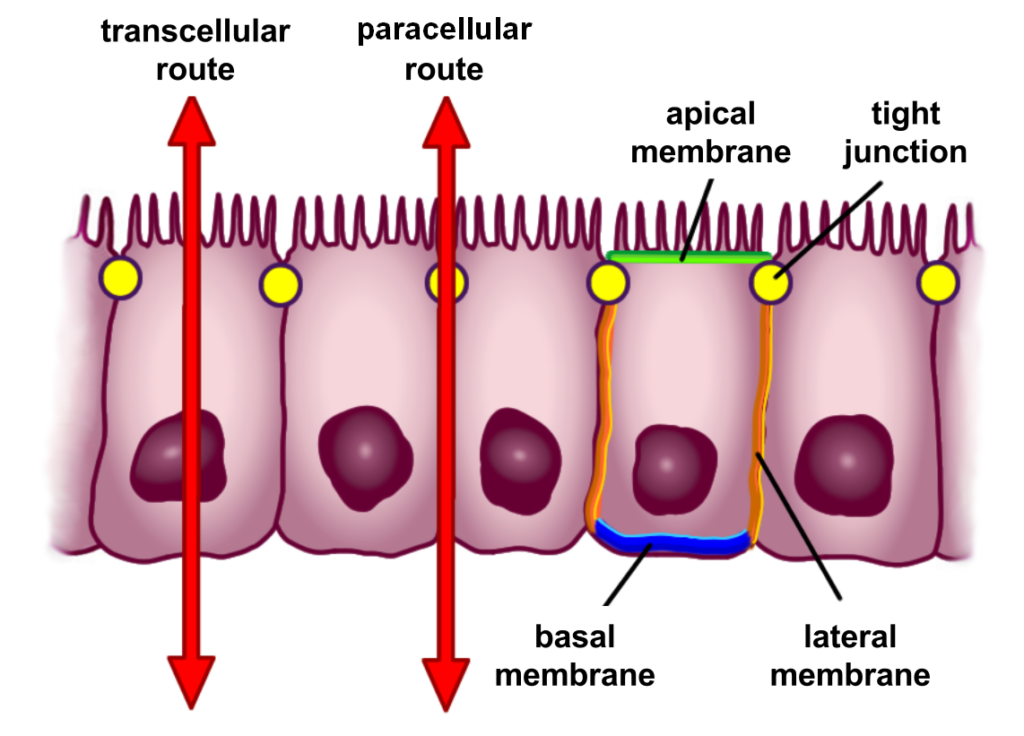
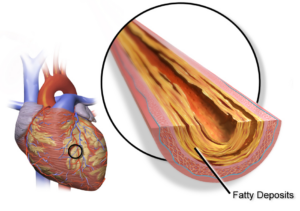
Atherosclerosis is the buildup of plaque on the endothelial cells lining the interior surfaces of your veins, arteries, and capillaries. It occurs when the cell wall is damaged through many mechanisms, which will be discussed later.
When low-density lipoprotein (LDL) can travel through the space created, it gets oxidized. When this occurs, our body’s natural response is to remove these oxidized LDL through phagocytosis, which is when white blood cells, in this case macrophages, engulf the oxidized LDL and attempt to remove it. When this occurs too frequently and with intensity, the body’s ability to clear this molecule eventually becomes compromised, and we accumulate these macrophages, leading to the development of foam cells. Foam cells attract platelets to the injury site and create a thrombus.
This may be challenging to understand, but when the cell lining is damaged, our ability to clear the damage becomes compromised, and we build up undesirable plaque that narrows the small veins in our body called venules.
What are the Mechanisms?
When we think about the buildup of stiffness and plaque within the endothelial lining, we assume cholesterol or LDL is the culprit. It does play a role, but the damage to the wall is the first stage of dysfunction within the system. Understanding why this occurs and correcting it is just as important as lowering LDL. Here are the mechanisms:
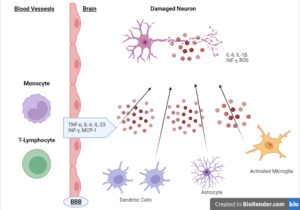
Inflammation and Oxidative Stress. Without doing a deep dive into these mechanisms, understand that inflammation and oxidative stress are the low-grade simmering fires occurring in the body without strong symptoms. They occur for many reasons, including obesity, smoking, trans fats, alcohol, and poor diet. When left unchecked or without counterbalances, they damage the cell lining, initiate an “inflammasome” response, and create the first steps for atherosclerosis. Both have also been shown to lower the body’s nitric oxide levels.
High Blood Pressure. As discussed in the blood pressure protocol, high blood pressure is one of the leading causes of heart-related issues and, when left unchecked, can be one of the major causes of arterial stiffness.
High blood pressure causes shear stress to the endothelial lining and must be addressed if optimal vascular health is to be achieved. See the blood pressure cheat sheet for more information on this topic.
Blood Sugar Dysregulation. When blood sugar becomes dysregulated, the increased circulating blood sugar can cause damage to the cell lining, increase systemic inflammation, and oxidize LDL. Elevated blood sugar has also been associated with lowering nitric oxide synthase. Nitric oxide synthase is responsible for producing nitric oxide, which helps break down atherosclerosis and the vasodilation of blood vessels.1
Low Nitric Oxide. Low nitric oxide may be due to the above mechanisms and is one of the early stages of dysfunction. Vasodilation of blood vessels isn’t the only role nitric oxide plays, but we will focus on it here.
Nitric oxide slowly lowers as we age and appears to run in concordance with atherosclerosis. 2 There has been a connection between nitric oxide production and vascular age – we are all seeking longevity, but do we know our vascular age?
Other Factors. In addition to direct insults, a multitude of other factors upstream may cause vascular damage. Pathogens such as H-pylori, poor oral and gut health, and poor hormonal health can all contribute to the advancement of atherosclerosis. Where you start your journey will depend on how far advanced the issue is. Knowing the first step is essential to stopping the spread quickly.
What are the Solutions?
There are many effective approaches to address arterial plaque. Here are four major ones:
1. Diet. The diet may be specific to the primary mechanism affecting you, but when we look at the research, it appears that high-fiber diets with increased monounsaturated fats (olive oil) and polyunsaturated fats (from fish oils) have the greatest benefit. Protein targets sit lower than expected and should be approximately 15-20% of the total daily intake from organic sources. This diet mimics a Mediterranean diet, and there is some evidence to suggest a plant-based diet can be of benefit here. However, some high-quality protein is necessary.
The key is eliminating all processed food, lowering sugar intake, and eating only whole foods. Lowering saturated fats to less than 10% of total fat is also essential.
Is there a place for fasting? Yes, there is evidence that fasting could be a positive intervention in cardiovascular disease. Some of the research from Dr Longo has shown positive outcomes and C-reactive protein, triglycerides, and LDL, all markers of cardiovascular risk.2
Introducing fasting mimicking or water-only fasting shows promise but must be addressed by a cardiologist.
Takeaways: Think of the plaque-reversal diet as a modified Mediterranean diet with increased fat from good sources, low-medium protein, and high fiber intake. Your plate should be half fruits and vegetables, a quarter high-quality meat and fat, and some grains. Fasting could be an adjunct that is used every quarter or six months.
2. Training. Boosting nitric oxide production and mitochondrial density through training can be a key modulator of overall health. However, your ability to output may be compromised if you already have advanced atherosclerosis, so finding the correct volume and intensity for you will be crucial to recovery. Training can do far more than just the mechanisms above; it can increase muscle mass, improve gut health, regulate blood sugar, and contribute to fat loss.3 As discussed in this study, the loss of muscle mass is strongly associated with cardiovascular disease.
Combining aerobic and higher-intensity training is the best approach for improving cardiovascular health. Here is an example of a training schedule for cardiovascular health:
- HIIT 2-3 times weekly. It increases the number of mitochondria and improves insulin sensitivity.
- Get VO2 to an exceptional level.
- Zone 2: 3 hours weekly MINIMUM as maintenance and 5-10 hours daily for faster progress.
- Doing this outside when possible is great for the mind and nervous system.
Takeaways: Training is one of the most important lifestyle modifiers for improving cardiovascular function. Anything is better than nothing, but attempting to track VO2 max and increasing it clearly indicates cardiac improvements.
3. Lifestyle. Lifestyle is often neglected when addressing cardiovascular risk. Sleep and stress management are the starting points and contribute to progression.
Sleep. Sleep has been shown to increase all risk factors for cardiovascular disease, including oxidative stress and inflammation.4 Sleep deprivation and loss can significantly affect blood sugar control, even when meals are controlled.5 Furthermore, lack of sleep has been associated with increased blood pressure and endothelial dysfunction.6
Stress. Research has mentioned stress as one of the major independent factors that can contribute to the creation and progression of atherosclerosis through the same mechanisms discussed above. One study regards stress as a potential patient zero of atherosclerosis.7
Takeaways: Creating a lifestyle change may be one of the central components of any heart-centric protocol, as follows:
- Creating appropriate sleep hygiene
- No food 3 hours before bed
- No work 2 hours before bed
- No screens 1 hour before bed
- Stress reduction methods must also be incorporated into the plan.
- Yoga
- Meditation
- Breathwork
4. Supplements. When breaking down the supplement plan for a plaque reversal guide, it is essential to understand that these are top-down approaches, meaning they will not deal with any specific issues outside that may be contributing, like endocrine dysfunction or infection. Here is a guide to supplement, along with hyperlinks on where to purchase them:
Fish Oil
Multiple studies have shown that fish oil benefits cardiovascular function, especially in higher doses. One study demonstrated that for every 1-gram increase in EPA/DHA, there is a 6 and 9% reduction in cardiovascular events and heart attack up to a dose of 5 grams.8 Dosage: Supplementing with up to 5 grams shows benefits. Do so in divided doses.
B-vitamins
Extensive studies have shown that B vitamins lower stroke risk. This is likely due to folate and B-12’s ability to lower homocysteine, a methylation marker, and high levels associated with cardiovascular and metabolic risk. Dosage: 1 capsule daily. The dose may need to be increased if you have genetic SNPs in MTHFR.
Let’s move on to more specific supplements:
Plant Sterols
Plant sterols are similar compounds to human cholesterol and compete with cholesterol in the body and have been shown to help lower cholesterol levels in humans.9 These can be taken in through diet or supplementation. Dosage: 3 tablets daily, in divided doses.
Pycnogenol and Centella Asiatica
The antioxidant and nitric oxide effects of this combination have been shown to halt the progression of atherosclerosis and, in one study, even showed a modest reversal.10 Dosage: 2 tablets daily in divided doses.
Resveratrol
Resveratrol is a polyphenol found in grapes, berries, and peanuts. Studies have shown it to stop the uptake of oxidized LDL and block the production of foam cells. Evidence suggests it can also have positive effects on blood pressure.11 Dosage: 3 grams daily of EPA/DHA in split doses.
Garlic extract
Although cholesterol is not the only factor contributing to atherosclerosis, it is necessary to lower total cholesterol and LDL if elevated when the damage is already done. Garlic extract and the allicin within it have been shown to affect the development of atherosclerosis, lower blood pressure, and lower total cholesterol and LDL.12 Dosage: 4 capsules daily, in divided doses.
Nattokinase
Nattokinase is an enzyme from a Japanese food called natto. It has been shown to affect blood coagulation or the thickness of the blood positively. Studies show that it has platelet-lowering effects and can lower fibrinogen, another cardiovascular risk marker. Ask your doctor if nottokinase is the right supplement for you if you have used blood thinners. Dosage: 1 capsule daily.
Neo40
Nitric oxide production is critical to endothelial health. Our ability falls as we age, but nitrites, found in beetroot extract, have been shown to positively affect nitric oxide production, without arginine and citrulline. The supplement above provides beetroot extract with vitamin C, which increases the ability to increase nitric oxide. Dosage: 2 tablets daily for one month, then one tablet daily.
Vitamin D and K
Vitamin D and K2, in particular, have been shown to positively affect the heart’s regulation and the arteries’ calcification. Vitamin K2 is responsible for calcium regulation in arteries and bones, and studies have shown that the combination has led to a slower progression of cardiovascular disease.13 Dosage: 1 tablet daily, with breakfast.
Chelation Therapy. Chelation therapy refers to an intravenous infusion of a compound called disodium ethylenediamine tetraacetic acid (EDTA). It binds to heavy metals in the body, and there is some evidence that it may benefit atherosclerosis. The science has been mixed and is not recommended by the American Heart Association; however, one study has shown promise,14 although the side effects of such therapy may not warrant experimentation.
Conclusion
Cardiovascular disease is multi-faceted and needs to be addressed by targeting multiple mechanisms. A generic protocol will aid in stabilizing coronary calcium, but specific targets may be warranted individually. Targeting the mechanisms above is a safe and effective starting point to ensure that you die with atherosclerosis and not because of it.
Reference Links :
1. https://pubmed.ncbi.nlm.nih.gov/29669543/
2. https:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6816332/
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6412503/
5. https://link.springer.com/article/10.1007/s00125-021-05608-y
7. https://pubmed.ncbi.nlm.nih.gov/34988123/
8. https://pubmed.ncbi.nlm.nih.gov/32951855/
9. https://pubmed.ncbi.nlm.nih.gov/25809853/
10. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613