What is it?
Attention Deficit Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that significantly impact an individual’s daily functioning and development.
ADHD typically begins in childhood and can persist into adolescence and adulthood. The core symptoms of ADHD can manifest in various ways and may include the following:
Inattention: Difficulty sustaining attention, being easily distracted, overlooking details, making careless mistakes, and struggling with organization and time management.
Hyperactivity: Restlessness, excessive fidgeting, difficulty remaining seated or quiet when expected, and a constant need for movement or activity.
Impulsivity: Impulsivity involves acting without thinking, having difficulty waiting for turns, interrupting others, blurting out answers, and engaging in risky behaviors without considering the consequences.
The severity and combination of ADHD symptoms can vary among individuals, leading to different presentations of the disorder. Here are the three main subtypes of ADHD recognized in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5):
1. Predominantly Inattentive Presentation: Characterized by inattention without significant hyperactivity-impulsivity.
2. Predominantly Hyperactive-Impulsive Presentation: Characterized by hyperactivity-impulsivity without significant inattention.
3. Combined Presentation: Characterized by inattention and hyperactivity-impulsivity.
ADHD can have significant functional impairments in various areas of life, including academic performance, social interactions, work, and relationships. It can also be associated with coexisting conditions, including learning disabilities, mood disorders, anxiety disorders, and substance use disorders.
Effective management of ADHD typically involves a multimodal approach tailored to individual needs, which may include medication, behavioral therapy, educational interventions, and support services. Early diagnosis and intervention are essential for minimizing the impact of ADHD symptoms and improving long-term outcomes.
What are the mechanisms?
This is where the difficulty arises when looking at the mechanisms of ADHD. There is the brain-centric approach to ADHD and the brain’s inability to produce dopamine and the downregulation of dopamine receptors. This is what I would regard as the outcome of ADHD – now let’s look at the causes of this downregulation:
Oxidative Stress. Although early in its research, oxidative stress appears to play an integral role in the severity of ADHD patients, and markers of oxidative stress are elevated in most studies.1 Oxidative stress is a natural byproduct of energy production in the mitochondria. However, when it is not quelled by enough antioxidants, either in the body or from external intake, it can cause cell damage, signaling issues, and lower dopamine production in the brain.
Mitochondrial Dysfunction. A knock-on effect of oxidative stress is poor mitochondrial function. If you remember biology from school, the mitochondria are thought of as the energy “powerhouse” of the cell where the majority of ATP is created, which is the body’s energy currency. Increased oxidative stress leads to poor production of energy within the cell and causes poor energy availability to the brain, leading to increased symptoms of ADHD. Again, the research is still in its infancy, but it does appear to have a clear role.2
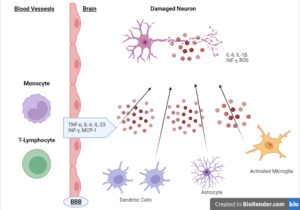
Neuroinflammation. Inflammation is a process that occurs throughout the body and is a known part of the triad of mito dysfunction-oxidative stress-inflammation. This cycle can run in any direction, and one exacerbates the other, but the idea of neuroinflammation is a more recent discussion with ADHD. An increase in low-grade inflammation in the brain can have an association with many neuropsychological issues, including autism, schizophrenia, and, more recently, ADHD. An increase in neuroinflammation can cause increased ADHD symptoms.3
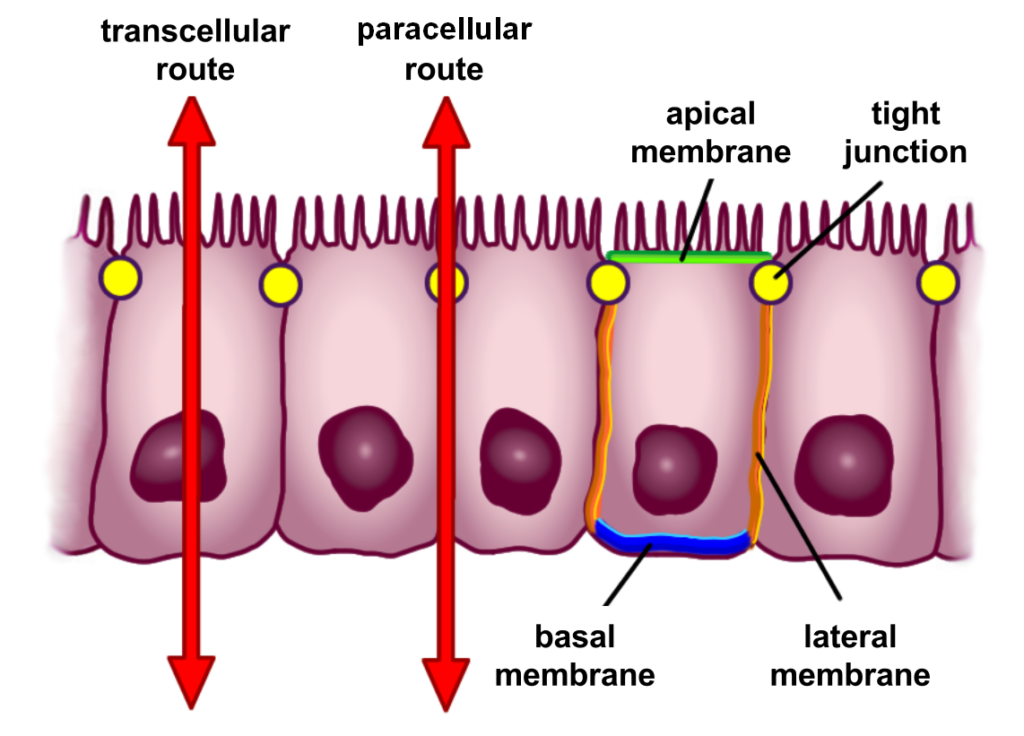
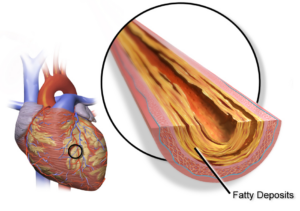
Gut Health. This is one of the more nuanced subjects when it comes to ADHD, as gut health issues are common comorbidities. The relationship between the gut and the brain is an area of continued research, but studies indicate that increased gut permeability, or leaky, is correlated with ADHD symptoms.4
Probiotics have positive effects on ADHD symptoms. In one study, probiotic supplementation improved immune markers and increased butyrate production in ADHD children.5 In my opinion, increased dysbiosis, intestinal permeability, and endotoxemia are associated with ADHD and have been linked to other neuropsychiatric conditions.
What are the solutions?
Changes in diet, training, lifestyle, and the use of supplements have shown promise in addressing ADD/ADHD. Let’s examine each of them.
Diet. Dietary approaches have been studied in ADHD, but they are limited. Removing processed food in one had positive effects, and a high-fiber DASH diet showed promise.6 Also, the use of an anti-inflammatory Mediterranean diet also shows promise.
There is some evidence to suggest that specific food coloring may have adverse effects on ADHD symptoms, although the research is rather old.7 Those with ADHD have also been shown to have a much higher prevalence of coeliac disease and other non-coeliac gluten intolerance.8 High-sugar diets have also been associated with increased ADHD symptoms, and although the science is conflicting, blood sugar control may improve neuropsychiatric symptoms.
According to the research, a whole-food diet with lower sugar and possible gluten removal is a reasonable approach to limiting ADHD symptoms. This is most likely due to the lowering of blood sugar spikes, the removal of inflammatory foods, and the removal of food triggers.
Training. Exercise has been shown to have significant effects on symptoms of ADHD, even after just one exposure. It increases executive function and focus on children exposed to aerobic training.9 Even in adults, a single bout of aerobic exercise for 20 minutes positively affected ADHD symptoms, showing that this may be an appropriate mode of exercise to control symptoms.10 One meta-analysis showed aerobic, steady-state training to be the most positive for working memory against other modes of exercise.11
The studies above show that training increases dopamine, attention, and BDNF, leading to improvements. It is also possible that aerobic exercise has positive effects on mitochondrial function, leading to improvements. I could not find research to back this hypothesis. However, aerobic exercise has been shown in the general population to increase total mitochondria and function.
There seems to be limited evidence for the use of strength training for ADHD, although it would most likely have benefits.
Lifestyle. Many lifestyle factors can affect the symptomatology of ADHD. Let’s look at two of them:
Sleep. One study showed that improvements in sleep hygiene positively affected sleep in ADHD children, leading to improvements in daily function, memory, and overall well-being. Over 25 percent of those with ADHD have some variation of sleep disturbance in combination, which can further exacerbate the condition. Looking at ways to improve sleep quality can be a significant leaver to pull in its treatment.
Cognitive Behavior Therapy. CBT is the most effective psychological treatment for ADHD in adults. It has been shown to have positive effects on depression, anxiety, and long-term outcomes.12
Supplements. Standardized nutrient deficiencies need to be addressed before you add anything specific to a plan for ADHD. I will discuss these first.
Vitamin D Vitamin D is lower in children with ADHD, and many studies have shown that vitamin D can have positive effects on executive function and impulsivity.13 Vitamin D is a simple and cheap approach to improving symptoms. The most significant improvements were shown in those with the lowest levels, so getting a standard vitamin D test is beneficial. Dosage: 5000-10000IU daily, depending on vitamin D levels.
Zinc Zinc has also been shown to be low in children with ADHD, and the use of it supplementally has been shown to have positive effects in combination with stimulant medication.14 Dosage: 30mg daily for eight weeks.
CoQ10 As with zinc, CoQ10 was used with standard care, improving symptoms and lowering side effects. As mentioned in the mechanism section, mitochondrial dysfunction may be one reason for ADHD, and CoQ10 is one of the nutrients needed for proper function. Dosage: 200mg daily in split doses.
MultivitaminNutrient deficiencies have been seen in ADHD patients, and the use of multivitamins has shown positive outcomes in the same population. One study on adults using multivitamins showed positive effects on depressive symptoms in ADHD patients.15 Dosage: 4 tablets in split doses.
FIsh Oil Although the research on fish oil is mixed, this may be due to using different dosages in studies. I would suggest the use of fish oil in ADHD as it plays a role in controlling inflammation, and that is part of the mechanisms discussed above. Dosage: 4 tablets a day, in split doses.
Now that we have covered the basics, we can examine some other speculative supplements that could be involved.
Probiotics. Again, the gut and the brain are intimately connected, and probiotics have been shown to affect many brain conditions, including depression.16 Although the research on their effects on ADHD is limited, the same mechanism remains, and there is some evidence to suggest it can be beneficial there, too. One study showed benefit in symptoms17 while others show that mothers using probiotics have an association with less likelihood of ADHD in their children. Dosage: The type and dosage are more difficult to advise, as there are too many combinations to give standard advice.
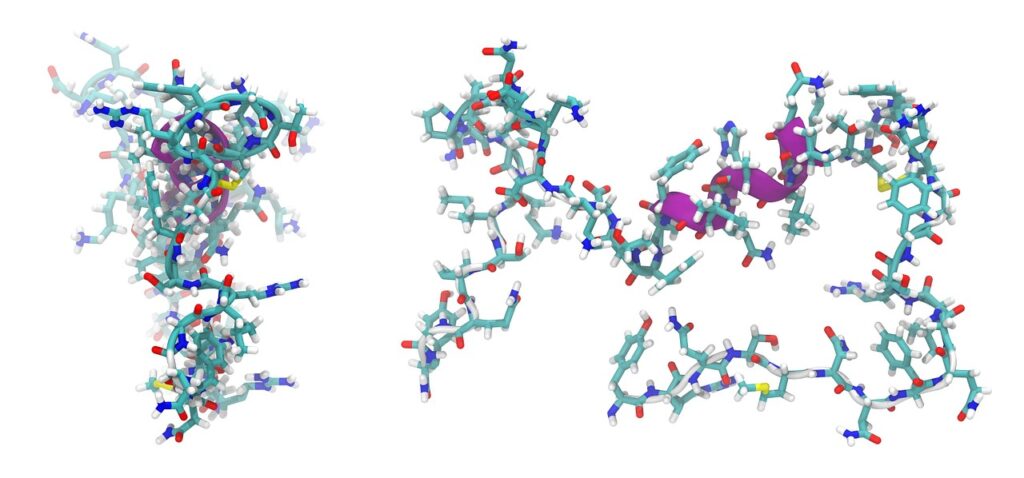
NAC N-acetyl cysteine has been shown to have a positive effect on many neurological conditions, like depression, anxiety, and schizophrenia. This is due to its ability to regulate oxidative stress and inflammation. One study has shown it to affect symptoms of ADHD in those with lupus.18 Dosage: 1.5-2.5 grams daily, in divided doses.
Curcumin Similar to NAC, curcumin has been shown to have profound effects on depression and anxiety. Its use has been studied in ADHD but only in the animal model, so the research is very much in its infancy. 19 Although in its early stages, curcumin’s neuroprotective abilities could benefit ADHD in humans. Dosage: 1-2 grams daily in divided doses.
Pycnogenol. There is evidence that some compounds increase circulation and eNOS (endothelial nitric oxide) production in ADHD, and pycnogenol is one of those. It has been shown in some small studies to help control symptoms, and this may be due to its ability to increase nitric oxide and lower oxidative stress.19 Dosage: Doses are between 100 and 200mg in divided doses are adequate.
Conclusion
The research on the mechanisms and control of ADHD has expanded dramatically in recent years, and the holistic approach to management is very much accepted in the research. Challenging the mechanisms rather than controlling symptoms may be of great benefit to the overall well-being of ADHD patients.
Reference Links :
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7070894/
2. https://www.eajm.org/Content/files/sayilar/224/29.pdf
3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6855401/
4. http://www.ncbi.nlm.nih.gov/pubmed/30414552
5. http://www.ncbi.nlm.nih.gov/pubmed/36904292
6. http://www.ncbi.nlm.nih.gov/pubmed/32220366
7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9573786/
9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6945516/
10. https://www.nature.com/articles/s41598-019-56332-y
11. http://www.ncbi.nlm.nih.gov/pubmed/37033046
12. http://www.ncbi.nlm.nih.gov/pubmed/31189374
13. http://www.ncbi.nlm.nih.gov/pubmed/31368773
14. http://www.ncbi.nlm.nih.gov/pubmed/34184967
15. http://www.ncbi.nlm.nih.gov/pubmed/24482441
16. https://pubmed.ncbi.nlm.nih.gov/31004628/
17. http://www.ncbi.nlm.nih.gov/pubmed/35207715